We are near the end of July, and COVID-19 still is spreading uncontrollably in the Houston area. The public is bombarded daily with a slew of metrics: new cases, positivity rates, hospitalizations, deaths.
What do they all mean? Local government reporters Zach Despart and Mike Morris review this public data every day. We asked them to help you understand how to make sense of it all, starting with the question on everyone's mind: How bad is the situation now?
Mike Morris: Well, it’s not great. We’re still adding more cases than public health officials can keep up with, a fifth of all tests conducted for the virus across the region are coming back positive — a rate seven times higher than most of May — and many local hospitals are under tremendous strain, particularly in their intensive care units.
The good news is that overall COVID hospital admissions finally are falling, with the rate of ICU admissions roughly flat.
Zach Despart: The first thing to keep in mind is that in order to get the full picture, you have to look at several metrics together. And because there sometimes are lags in how the government reports data, resulting in single-day spikes, it’s best to look at seven-day trends.
Let’s start with cases. To see the daily counts, try the city-county COVID dashboard or the related Texas Medical Center chart. Our colleagues also track local and statewide metrics here.
Right now, the seven-day daily average of new cases in Harris County is 1,500. That’s high. To put that in perspective, Houston and Harris County health department contact tracers can handle about 600 cases a day.
Another data point is the number of tests that come back positive, which in the TMC system is at about 18 percent. On June 1, that figure was 5 percent. The governor’s team set 10 percent as a warning benchmark, which we exceeded a month ago.
Positive tests are called a leading indicator, which researchers can use to project hospitalizations and deaths. But it is an imperfect one; a limited ability for testing means that health experts believe the number of infections may be as much as 10 times greater than the documented figure.
Other metrics are more reliable.
MM: Hospitalizations are the best indicator of the virus’ spread, in large part because those with mild or no symptoms may never get tested or seek care, and, thus, may never show up in the data.
To gauge how the hospitals are doing, we look at two data sets: One is from the Southeast Texas Regional Advisory Council, also known as SETRAC, which covers the 25-county region anchored by Houston. The other is from the Texas Medical Center, which pulls data from every facility in the region that is affiliated with seven large hospital systems headquartered in the huge medical complex south of downtown. The TMC figures come primarily from Harris, Fort Bend and Montgomery counties.
On the SETRAC dashboard, you can see hospital beds in all 25 counties, or select one at a time. In Harris, only about half of the “operational” general beds are full, but that’s not a useful way to measure the strain caused by the virus. The most valuable resource — and the most limited one in a pandemic, when a lot of patients are severely ill at once — is space in intensive care units. And the data shows ICUs have been near capacity across the county for much of July.
We typically look at the TMC data on this “capacity” point; while the SETRAC data is interactive and shows a longer-term trend, the TMC data, while not perfect, more clearly spells out ICU capacity. (Here is the explanation of what the “phases” of surge capacity mean.) The institutions have had a few hiccups in conveying exactly how urgent their capacity challenges are, though.
ZD: Long story short, in late June the TMC executives warned ICU usage was increasing at an alarming rate. Then the CEOs walked back their statements. And then the ICU slides disappeared from the TMC’s online deck just after the system hit 100 percent of base capacity for the first time during the pandemic. Understandably, this alarmed some people, and we wrote a story about it. TMC replaced the data a few days later, removed the scary red and orange colors from the charts, and added context.
Does this switcheroo mean the data is untrustworthy, as some have suggested? Of course not. But some of the revised slides are wonky and require some explanation. Here are two we find particularly helpful.

MM: This chart on ICU occupancy is a graphic designer’s nightmare (spiky green boxes!), but it’s important. The column on the left shows the raw count of ICU patients (COVID patients and total patients, marked by yellow lines) and which “phase” of operations the combined count requires. TMC ICUs have been in “Phase 2” for most of July, adding staff and equipment to convert normal beds into intensive care beds.
Now, let’s look at the ovals listing percentages to the right. For much of July, COVID patients have made up roughly half of all medical center ICU patients (the oval at the bottom left). That’s a significant burden — the state and county warning benchmarks consider anything higher than 15 percent a red flag.
What about the lighter blue percentage ovals? Those figures try to convey the wiggle room provided by surge capacity. As of Friday, for instance, if all Phase 2 beds were added, the medical center ICUs would be 85 percent full, with 42 percent of all ICU beds filled with COVID patients.
Dr. Marc Boom, CEO of Houston Methodist, and Dr. Jim McDeavitt, dean of clinical affairs at Baylor College of Medicine, said they know the capacity slides can be hard to interpret.
“What we’re all seeing is people on either extreme trying to use data to prove their more extreme views, whether it’s somebody looking at that and saying, ‘There’s no problem, look at all these beds,’ or frankly people looking at, ‘Oh my gosh we’ve gotten through Phase 1, the sky is falling,’” Boom said. “Both of those are wrong.”
If the dark blue of Phase 1 is your favorite restaurant on a Wednesday night, McDeavitt said, the sky blue of Phase 2 is that restaurant on Mother’s Day.
“When we get up into the light blue zone (Phase 3), that’s when we start to deliver care in a way nobody really wants to, like putting two beds in one room or putting beds into places in a hospital where we wouldn’t normally put beds,” McDeavitt said.
And that gray box at the top? “Armageddon,” McDeavitt said. “We have medical ships showing up in the port of Houston.” That scenario, Boom agreed, would be like New York City in March. The gray box, he said, “certainly is not meant to reassure people that there’s some endless supply of beds.”
One last thing to note here is that this ICU capacity data is aggregated from multiple facilities, and that not every hospital has the same ability to add “surge” beds. For example, Harris County’s public safety net hospitals have regularly reported ICU usage above 100 percent during the pandemic and continue to transfer patients to other facilities due to a lack of space.

A lot of people have focused on this projection slide, but it’s not a crystal ball. It’s a simple calculation: If ICUs continue to be this full, how quickly will the TMC enter its two phases of surge capacity at the current rate of COVID ICU admissions?
Hospitals have some control over one part of that equation: The numbers of non-COVID patients in intensive care, many of whom are there to recover from procedures that can be delayed. We saw this play out this month: TMC ICUs were initially projected to enter Phase 3 (formerly dubbed “unsustainable surge capacity”) within two weeks, but that date always stayed 12 to 13 days away.
There are two reasons for this: The count of non-COVID patients fell 16 percent between July 2 and July 5 as procedures were postponed, and has not returned to its early-July levels. And that was followed by two weeks during which the 7-day average growth in COVID ICU cases slowed every day.
ZD: And here’s a brief primer on the SETRAC data. We primarily look at three data points: COVID cases occupying general beds, those in ICU beds and total ICU usage.
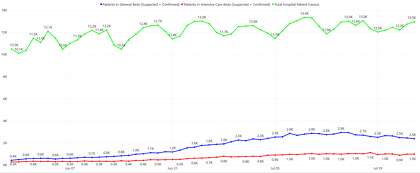
This graph shows how many COVID patients are hospitalized in the 25-county region, split between general beds (blue) and the portion of those that are in the ICU (red). There are thousands of general beds available across the region, though that figure still is useful because it helps predict future ICU usage. Why? Because some of those people, unfortunately, get sicker and need intensive care.
The number of ICU patients is of particular concern, because those resources are more limited.

This chart shows the total ICU usage in the region (blue) and the share of those patients that are being treated for COVID (green). As you can see, we’ve been pretty close to using up all the base ICU capacity since early June. And remember, this is an average of dozens of hospitals; some are into their surge capacity while others are below it.
The second marker to watch here is the share of ICUs that are filled with COVID patients. Under the state benchmark, this figure should be no higher than 15 percent; for more than a month it has been above 40 percent. Why is this concerning? COVID patients need to be isolated from others and require more staff attention and supplies, such as PPE, than other ICU cases.
And some of these ICU patients die, bringing us to our last data point.
MM: What’s helpful to understand is that these metrics increase in succession. In June we saw an increase in cases after the state began to reopen. In late June and early July, hospitalizations surged. Mid-July, predictably, has brought an increase in deaths. Harris County has reported 596 fatalities to date, while the state has tallied 4,717. Most have come since June. (You can find these stats in the statewide data dashboard.)
The statewide death rate as a share of total cases, however, is quite low — just 1.2 percent, well below the 7.7 percent rate in New York, which was battered by the virus in the spring.
Why is that? Three primary reasons: the Texans who made up the recent case surge often were younger and more capable of fighting off the disease, doctors have gotten better at treating it over the past six months, and many of the patients who are among the recent surge in cases are still fighting the disease — it is inevitable that a portion of them will die. Some critics of Texas’s coronavirus restrictions — including a brief stay-at-home order and current mask rules — point to the low death rate as evidence those measures were unneeded.
Doctors stress it’s important to consider that the outcomes of a COVID infection aren’t binary; that is, life or death. McDeavitt said he is confident that once intensive studies are completed on the lasting damage the virus does to the body, researchers will find “non-trivial” percentages of patients with permanent lung damage, with cognitive impairments, and with heart attacks, strokes and other maladies caused by blood clots.
ZD: These data sets, while sometimes hard to read, are valuable for us and the public to understand the spread and severity of the COVID-19 pandemic here. Feel free to ask us questions via email or Twitter, and continue to follow the Chronicle’s coronavirus coverage.
zach.despart@chron.com
mike.morris@chron.com
"how" - Google News
July 26, 2020 at 06:00PM
https://ift.tt/3jIIZbR
So, how bad is COVID-19 in Houston? A guide to reading the data - Houston Chronicle
"how" - Google News
https://ift.tt/2MfXd3I
Bagikan Berita Ini














0 Response to "So, how bad is COVID-19 in Houston? A guide to reading the data - Houston Chronicle"
Post a Comment